Navigating the medical device approval process is a complex journey, demanding meticulous planning and rigorous adherence to regulatory guidelines. This process, vital for ensuring patient safety and efficacy, involves a multifaceted approach encompassing pre-market activities, rigorous testing, and ongoing post-market surveillance. Understanding the intricacies of this process is crucial for both manufacturers and healthcare professionals alike, impacting everything from product development timelines to market access strategies.
This guide aims to demystify the complexities, providing a clear and concise overview of each critical stage.
From initial concept to final market release, the approval process demands a deep understanding of various regulatory pathways, including 510(k) clearance, PMA approval, and De Novo classification. Each pathway presents unique challenges and opportunities, requiring tailored strategies to ensure compliance and timely market entry. Beyond regulatory compliance, the process also emphasizes ethical considerations, risk management, and the critical role of post-market surveillance in maintaining product safety and efficacy throughout the device’s lifecycle.
This guide explores these aspects in detail, offering valuable insights for anyone involved in the development and commercialization of medical devices.
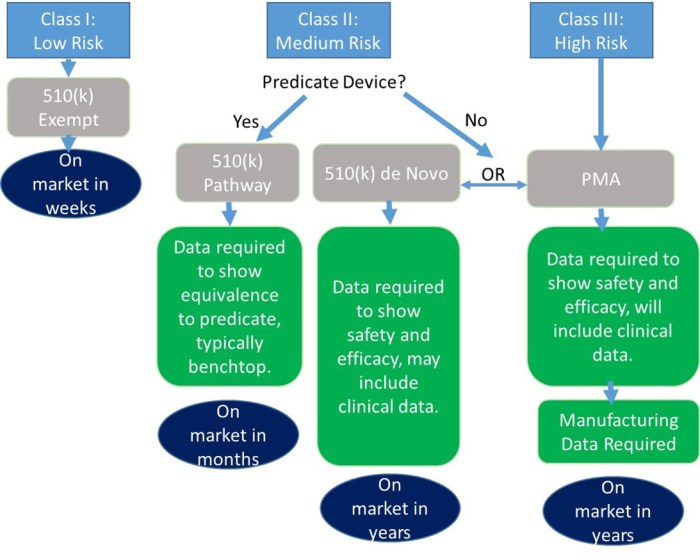
Regulatory Pathways for Medical Device Approval
Navigating the regulatory landscape for medical devices in the United States involves understanding the different pathways available for obtaining market authorization. The choice of pathway significantly impacts the time, cost, and complexity of the approval process. This section Artikels the key differences between the three primary pathways: 510(k) clearance, Premarket Approval (PMA), and De Novo classification.
510(k) Clearance
The 510(k) pathway is used to demonstrate that a new medical device is substantially equivalent to a legally marketed predicate device. This means the new device has the same intended use and comparable safety and effectiveness as the predicate. This is the most common and generally fastest route to market. Examples of devices cleared through this pathway include many types of diagnostic tests, simple surgical instruments, and certain types of wound dressings.
The requirements include submitting a detailed 510(k) premarket notification to the FDA, including data demonstrating substantial equivalence. Pre-submission meetings with the FDA are often helpful to clarify requirements and address potential issues early in the process. Post-market surveillance is generally less stringent than for PMA devices, but manufacturers are still responsible for monitoring device performance and reporting adverse events.
Premarket Approval (PMA)
Premarket Approval (PMA) is the most rigorous pathway and is required for high-risk devices where substantial equivalence cannot be demonstrated. This process involves extensive clinical trials to demonstrate the safety and effectiveness of the device. Examples of devices requiring PMA include implantable cardiac devices, some types of surgical robots, and complex life-support systems. The requirements for PMA are considerably more demanding than for 510(k) clearance.
They involve detailed pre-submission meetings with the FDA, rigorous testing protocols including extensive clinical trials, and comprehensive post-market surveillance. This includes detailed reporting of adverse events and regular follow-up on device performance.
De Novo Classification
The De Novo pathway is used for devices that are novel and do not have a legally marketed predicate device. This pathway provides a clear regulatory pathway for these innovative devices. Examples include certain types of novel drug delivery systems and advanced imaging technologies. The requirements for De Novo classification involve submitting a detailed submission package to the FDA demonstrating the safety and effectiveness of the device, often including clinical data.
Similar to PMA, pre-submission meetings are highly recommended. Post-market surveillance requirements are generally comparable to PMA, reflecting the inherent risks associated with novel technologies.
Comparison of Regulatory Pathways
The following table summarizes the key differences between the three pathways:
| Pathway | Requirements | Timeline (Estimated) | Cost (Estimated) |
|---|---|---|---|
| 510(k) | Demonstrate substantial equivalence to a predicate device; pre-submission meetings optional; limited testing; less stringent post-market surveillance. | 6-12 months | $50,000 – $200,000 |
| PMA | Extensive clinical trials; rigorous testing; comprehensive post-market surveillance; mandatory pre-submission meetings. | 2-5 years | $1 million – $5 million+ |
| De Novo | Demonstrate safety and effectiveness of a novel device; rigorous testing; comprehensive post-market surveillance; mandatory pre-submission meetings. | 1-3 years | $500,000 – $2 million+ |
*Note: Timelines and costs are estimates and can vary significantly depending on the specific device, complexity of the submission, and interactions with the FDA.*
Pre-Market Activities and Documentation
Successfully navigating the medical device approval process hinges significantly on thorough pre-market activities and meticulous documentation. These activities lay the groundwork for a robust submission, minimizing delays and increasing the likelihood of a positive outcome. This section details the crucial steps involved in preparing for regulatory submission.Pre-clinical studies are essential for demonstrating the safety and efficacy of a medical device before it’s tested on humans.
These studies provide critical data to support the claims made in the regulatory submission. They also help identify potential risks and refine the design of the device before it enters clinical trials.
Pre-clinical Study Design and Execution
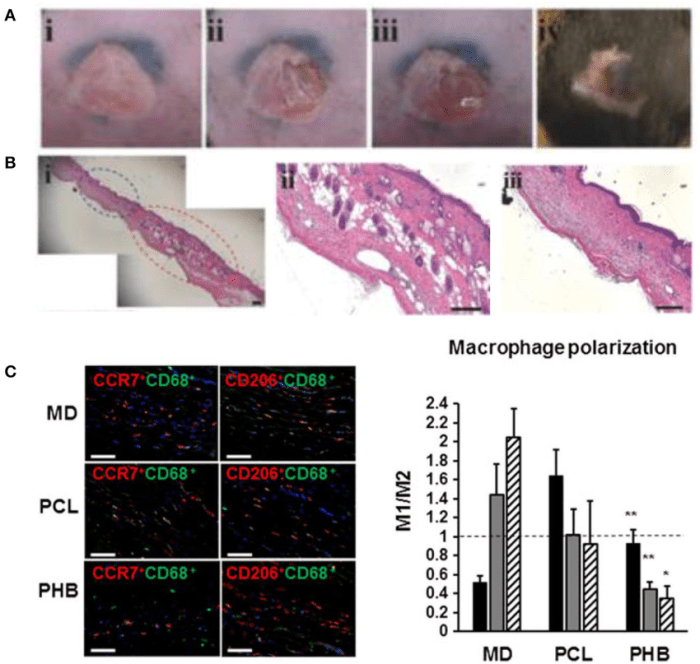
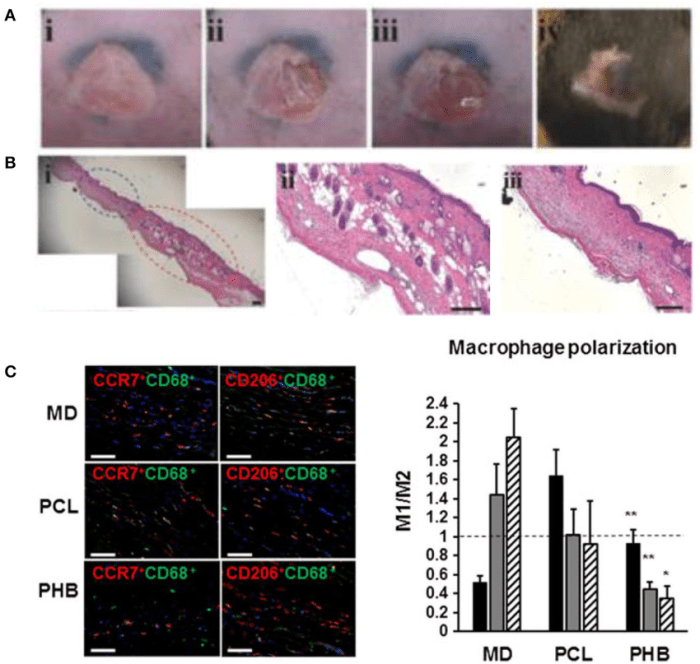
Pre-clinical studies typically involve in vitro (laboratory) and in vivo (animal) testing. In vitro studies might include biocompatibility testing (evaluating the device’s interaction with biological systems), mechanical testing (assessing strength, durability, and functionality), and chemical characterization (analyzing the device’s composition). In vivo studies often involve animal models to assess the device’s efficacy and safety in a living organism. Data analysis for pre-clinical studies involves statistical methods to determine the significance of the results, including techniques like t-tests, ANOVA, and regression analysis.
For example, a biocompatibility study might use statistical analysis to compare the cellular response to the device material versus a control material. Similarly, an in vivo study might use statistical analysis to compare the therapeutic effect of the device to a placebo or existing treatment.
Risk Management and Quality Systems
A robust risk management plan and a comprehensive quality system are critical throughout the entire medical device development lifecycle. Risk management involves identifying, analyzing, and mitigating potential hazards associated with the device. This process often employs techniques such as Failure Mode and Effects Analysis (FMEA) and Hazard Analysis and Critical Control Points (HACCP). A quality system ensures that the device is consistently manufactured to meet specified requirements and maintains its quality and safety.
- Design Control: A systematic approach to design, develop, and verify the device’s design.
- Manufacturing Process Validation: Ensuring the manufacturing process consistently produces a high-quality product.
- Quality Control: Implementing procedures to monitor and control the quality of materials, processes, and products.
- Corrective and Preventive Actions (CAPA): A system for identifying, investigating, and correcting quality issues.
- Document Control: Managing and controlling all documents related to the device’s design, manufacture, and quality.
- Supplier Management: Selecting and managing suppliers to ensure they meet quality requirements.
- Audits: Regular internal and external audits to assess compliance with regulatory requirements and quality standards.
Medical Device Submission Dossier Creation
Creating a comprehensive medical device submission dossier is a multi-step process requiring meticulous attention to detail. A well-organized dossier significantly increases the chances of a successful regulatory review. The dossier should be structured according to the specific requirements of the relevant regulatory agency (e.g., FDA, EMA).
- Planning and Preparation: Define the scope of the submission, identify the relevant regulatory requirements, and assemble the necessary team.
- Data Collection and Compilation: Gather all relevant data from pre-clinical studies, design documentation, manufacturing processes, and quality systems.
- Dossier Structure and Content: Organize the data according to the regulatory agency’s submission guidelines, ensuring clarity and completeness.
- Review and Validation: Conduct thorough internal reviews to ensure the dossier is accurate, complete, and consistent.
- Submission: Submit the dossier electronically or physically, depending on the regulatory agency’s requirements.
Submission Dossier Flowchart
A flowchart depicting the key stages of creating a medical device submission dossier would show a linear progression, starting with “Planning & Preparation,” followed by “Data Collection & Compilation,” then “Dossier Structure & Content,” leading to “Review & Validation,” and finally culminating in “Submission.” Each stage would be represented by a distinct box, with arrows connecting them to illustrate the sequential nature of the process.
The flowchart would clearly show the dependence of each stage on the preceding one. For example, the “Data Collection & Compilation” stage cannot begin until the “Planning & Preparation” stage is complete. Similarly, the “Submission” stage cannot occur until the dossier has been thoroughly reviewed and validated.
Post-Market Surveillance and Reporting
Post-market surveillance (PMS) is a critical component of medical device regulation, ensuring the continued safety and effectiveness of devices after they’ve been approved for market use. It’s a proactive approach that complements pre-market assessments, allowing for the identification and mitigation of potential risks that may not have been apparent during the initial approval process. This ongoing monitoring is essential for protecting patients and maintaining public confidence in the medical device industry.Post-market surveillance activities encompass a range of strategies designed to gather information on device performance in real-world settings.
These activities are crucial for detecting unexpected adverse events, evaluating the long-term effectiveness of devices, and identifying areas for potential improvement in design or manufacturing.
Post-Market Surveillance Activities
A variety of methods are employed to conduct effective post-market surveillance. These include reviewing data from post-market studies, analyzing reports of adverse events, conducting periodic inspections of manufacturing facilities, and actively soliciting feedback from healthcare professionals and patients. Data analysis from large registries, combining information from multiple sources, can provide valuable insights into device performance and potential safety signals.
For instance, a PMS program for a new cardiac implant might involve collecting data on patient outcomes, such as implant failure rates and the incidence of adverse events like infection or thrombosis, from multiple hospitals across the country. This aggregated data would be analyzed to identify any trends or patterns that might indicate a safety concern.
Adverse Event Reporting Procedures
Manufacturers, healthcare professionals, and patients all play a vital role in reporting adverse events associated with medical devices. The timely and accurate reporting of such events is crucial for identifying potential safety hazards and implementing appropriate corrective actions. Failure to report can have serious consequences for patient safety. The following table Artikels the key aspects of adverse event reporting:
| Reporter | Reporting Procedure | Timeframe |
|---|---|---|
| Manufacturer | Manufacturers are legally obligated to report any adverse events they become aware of, usually through a dedicated reporting system to the relevant regulatory agency. This often involves detailed documentation of the event, including patient demographics, device information, and the circumstances surrounding the event. | Generally, within a specified timeframe (often 24-72 hours for serious events) of becoming aware of the event. |
| Healthcare Professional | Healthcare professionals should report any suspected adverse events related to medical devices to the relevant regulatory agency. Reporting mechanisms vary depending on the country and the specific agency. Many countries have established online reporting systems to facilitate this process. | Generally, as soon as possible after the event is suspected. |
| Patient | While patients may not have access to the same level of detail as healthcare professionals, they can still report suspected adverse events to their healthcare provider or directly to the relevant regulatory agency. This often involves providing information about their experience with the device. | As soon as possible after experiencing the event. |
Regulatory Agency Oversight
Regulatory agencies such as the FDA (in the United States) and the EMA (in Europe) play a crucial role in overseeing post-market surveillance. They establish regulations, collect and analyze reports of adverse events, and take appropriate actions when necessary. This includes conducting investigations, issuing safety alerts or recalls, and updating regulatory requirements. Agencies actively monitor trends and patterns in reported adverse events to identify potential safety issues that may require immediate attention.
For example, if a significant increase in the number of reported malfunctions is observed for a particular device, the agency may initiate an investigation to determine the cause and recommend corrective actions.
International Medical Device Regulations
Navigating the global landscape of medical device regulation requires a thorough understanding of the diverse requirements and processes in major markets. Significant variations exist between regulatory bodies, impacting timelines, costs, and the overall approval process. This section will compare and contrast the key regulatory pathways in the United States, Europe, and Canada, highlighting the challenges and opportunities inherent in achieving global market access.
Comparison of US, European (CE Marking), and Canadian Medical Device Approval Processes
The regulatory pathways for medical device approval differ significantly across the US, Europe (with CE Marking indicating conformity with EU directives), and Canada. The US Food and Drug Administration (FDA) employs a risk-based classification system, categorizing devices based on their intended use and potential risks. This system dictates the level of premarket scrutiny, ranging from premarket notification (510(k)) for devices substantially equivalent to already-approved products, to premarket approval (PMA) for high-risk devices requiring extensive clinical data.
The European Union utilizes a system based on the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), with classifications based on risk and requiring conformity assessment procedures, leading to the CE mark. In Canada, Health Canada follows a similar risk-based approach, with licensing requirements varying depending on the classification of the device.
| Feature | United States (FDA) | European Union (CE Marking) | Canada (Health Canada) |
|---|---|---|---|
| Classification System | Risk-based (Class I, II, III) | Risk-based (Class I, IIa, IIb, III) | Risk-based (Class I, II, III, IV) |
| Approval Pathways | 510(k), PMA, De Novo | Conformity assessment procedures (Notified Bodies involved) | Licensing based on risk classification |
| Timeline | Highly variable, ranging from months to years | Highly variable, influenced by Notified Body workload and complexity | Variable, dependent on device complexity and regulatory interactions |
| Key Requirements | Premarket submissions, clinical data (depending on classification), quality system regulations (QSR) | Technical documentation, conformity assessment, clinical evaluation, post-market surveillance | Compliance with medical device regulations, quality management system (QMS), clinical data (depending on classification) |
Challenges and Opportunities in Obtaining Global Regulatory Approvals
Securing global regulatory approvals presents considerable challenges. These include navigating diverse regulatory requirements, managing significant costs associated with multiple submissions, and coordinating complex timelines across different jurisdictions. Harmonization efforts, while ongoing, are not fully realized, leading to inconsistencies and redundancies. However, successful global approvals open significant opportunities, including access to larger markets, increased revenue potential, and enhanced brand recognition.
A well-defined regulatory strategy, proactive engagement with regulatory bodies, and investment in robust documentation are crucial for mitigating challenges and capitalizing on opportunities. For example, a company might leverage a successful FDA approval to expedite the approval process in other countries, demonstrating a strong regulatory history.
Role of International Standards Organizations (e.g., ISO) in Harmonizing Medical Device Regulations
International standards organizations, such as ISO, play a vital role in harmonizing medical device regulations globally. They develop consensus-based standards that define requirements for quality management systems, risk management, and other aspects of medical device development and manufacturing. Adherence to these standards can facilitate regulatory approval processes, reducing the burden on manufacturers and promoting greater consistency across different jurisdictions.
For instance, ISO 13485:2016 provides a framework for quality management systems specific to medical devices, widely recognized and accepted by regulatory bodies worldwide. This harmonization simplifies the process, reducing the need for extensive modifications to meet diverse national standards.
Impact of Medical Research and Services on Device Approval
The approval of new medical devices is inextricably linked to advancements in medical research and the landscape of medical services. Research fuels innovation by providing the scientific foundation for new technologies, while the needs identified within healthcare systems drive the development of solutions. The interplay between these two forces shapes not only the creation of devices but also their eventual regulatory pathways and market adoption.Medical research directly influences the development and approval of new medical devices through the generation of evidence supporting safety and efficacy.
This evidence is crucial for navigating the regulatory hurdles imposed by agencies like the FDA (in the US) and its international counterparts. Without robust research, demonstrating the clinical benefits and minimizing potential risks becomes extremely challenging, potentially delaying or even preventing approval.
Advancements in Medical Research and Device Development
Significant advancements in areas like biomaterials science, nanotechnology, and imaging technologies have directly translated into new medical devices. For example, the development of biodegradable polymers has enabled the creation of resorbable stents, minimizing the need for a second procedure to remove them. Similarly, advancements in microelectronics have led to the development of smaller, more powerful implantable devices with improved functionalities, such as advanced pacemakers and insulin pumps.
The refinement of 3D printing techniques has opened avenues for personalized medical devices tailored to individual patient anatomy. These examples illustrate how fundamental research breakthroughs translate into tangible improvements in medical technology.
The Role of Medical Services in Identifying Unmet Clinical Needs
Medical services play a critical role in identifying unmet clinical needs that serve as the impetus for medical device innovation. Healthcare professionals working directly with patients are often the first to recognize gaps in existing treatments and technologies. These observations drive the demand for new solutions.
- The increasing prevalence of chronic diseases like diabetes has fueled the development of advanced insulin delivery systems and continuous glucose monitoring devices.
- The need for minimally invasive surgical techniques has driven innovation in robotic surgery and laparoscopic instruments.
- The limitations of traditional imaging modalities have spurred the development of advanced imaging technologies such as MRI and PET scans, leading to improvements in diagnostic capabilities.
- The challenges associated with managing heart failure have resulted in the development of sophisticated cardiac assist devices and implantable cardioverter-defibrillators (ICDs).
Impact of Medical Service Accessibility on Device Adoption
The availability and accessibility of medical services significantly impact the adoption and utilization of approved medical devices. In regions with well-established healthcare infrastructures and widespread access to specialists, the uptake of new devices is generally faster. Conversely, limited access to healthcare, lack of trained personnel, or inadequate infrastructure can hinder the adoption of even the most beneficial medical devices.
For example, the introduction of telemedicine technologies has been particularly beneficial in areas with limited access to specialists, facilitating remote patient monitoring and diagnosis, which can also positively impact the usage of related devices. Conversely, a lack of sufficient training for healthcare professionals on the use of new devices can lead to underutilization or even inappropriate use, potentially compromising patient safety and efficacy.
Ethical Considerations in Medical Device Development and Approval
The development and approval of medical devices present a complex interplay of technological advancement and ethical responsibilities. Ensuring patient safety and upholding ethical principles throughout the entire lifecycle of a device, from initial design to post-market surveillance, is paramount. This requires a rigorous and transparent process that prioritizes the well-being of individuals and the integrity of the medical field.The ethical considerations involved are multifaceted and demand careful consideration at each stage.
These concerns extend beyond simply adhering to regulatory requirements and encompass a broader responsibility to act with integrity and prioritize patient welfare.
Patient Safety and Informed Consent
Patient safety is the cornerstone of ethical medical device development and approval. All phases, including design, testing, and marketing, must prioritize minimizing risks and maximizing benefits for patients. This involves rigorous testing to identify and mitigate potential hazards, using appropriate materials and manufacturing processes, and providing clear and accurate information to healthcare professionals and patients. Informed consent is crucial; patients must understand the risks and benefits associated with a device before agreeing to its use.
This necessitates clear and accessible language in patient information materials, ensuring that patients are fully empowered to make informed decisions about their treatment. Failure to obtain truly informed consent can lead to serious ethical breaches and legal ramifications. For example, a device trial failing to fully disclose potential side effects could be considered unethical and potentially illegal.
The Role of Institutional Review Boards (IRBs)
Institutional Review Boards (IRBs) play a vital role in ensuring the ethical conduct of medical device research and development. These independent committees review research protocols to ensure that the rights and welfare of human subjects are protected. IRBs assess the risk-benefit ratio of proposed studies, scrutinize informed consent procedures, and monitor the ongoing safety and well-being of participants.
Their oversight is crucial in preventing exploitation and ensuring that research is conducted ethically and responsibly. An IRB’s rejection of a research protocol, for instance, could halt a device’s development until ethical concerns are addressed, highlighting the crucial gatekeeping function IRBs provide. The IRB’s review process often involves detailed examination of the study design, methodology, and data analysis plans to ensure scientific rigor and ethical compliance.
Ethical Considerations in Device Design and Testing
The design and testing phases of medical device development necessitate careful consideration of ethical implications. Design choices must prioritize safety and effectiveness, avoiding unnecessary risks. Testing procedures should minimize harm to human subjects, employing appropriate animal models where possible, and utilizing robust statistical methods to ensure reliable results. For instance, the selection of materials used in a device must consider biocompatibility and potential allergic reactions.
Furthermore, rigorous testing protocols should be developed to identify and mitigate any potential risks associated with the device’s use. Ethical dilemmas might arise when balancing the need for thorough testing with the potential delays in bringing life-saving devices to market. This requires a careful balancing act between thoroughness and timely availability.
Ethical Considerations in Marketing and Sales
The marketing and sales of medical devices must be truthful and not misleading. Promotional materials should accurately represent the device’s capabilities and limitations, avoiding exaggerated claims or unsubstantiated benefits. Furthermore, there must be transparency regarding potential risks and side effects. Unethical marketing practices, such as targeting vulnerable populations with misleading information or offering incentives to healthcare professionals for prescribing a specific device, are unacceptable.
For example, exaggerating the effectiveness of a device in promotional materials could lead to patient harm and erode public trust in the medical device industry. Maintaining ethical marketing practices is vital for preserving public confidence and ensuring responsible use of medical devices.
Successfully navigating the medical device approval process requires a multifaceted approach, combining a thorough understanding of regulatory requirements, meticulous documentation, and a commitment to patient safety. This process, while demanding, is essential for ensuring the safety and efficacy of medical devices, ultimately benefiting both patients and healthcare providers. By adhering to rigorous standards and maintaining proactive post-market surveillance, manufacturers contribute to a landscape of innovative and trustworthy medical technologies.
The information provided in this guide serves as a foundation for navigating the complexities of this critical pathway, fostering responsible innovation and improving healthcare outcomes.
FAQ Section
What is the difference between a 510(k) and a PMA?
A 510(k) demonstrates substantial equivalence to a legally marketed device, requiring less rigorous testing. A PMA requires extensive clinical trials to demonstrate safety and effectiveness for novel devices.
How long does the approval process typically take?
The timeline varies significantly depending on the regulatory pathway and the complexity of the device. It can range from several months for a 510(k) to several years for a PMA.
What are the costs associated with medical device approval?
Costs vary widely depending on the pathway, device complexity, and testing requirements. Expect significant expenses for pre-clinical studies, clinical trials, regulatory submissions, and post-market surveillance.
What happens if a serious adverse event is reported post-market?
Manufacturers are legally obligated to report serious adverse events promptly to regulatory agencies. This may trigger investigations, corrective actions, or even product recalls.

